Hearing “prominent bronchovascular markings” in your X-ray or CT report can sound alarming, but in most cases, it is a descriptive observation rather than a diagnosis. For some, it reflects temporary changes from an infection; for others, it may hint at chronic lung or heart issues that need monitoring. The best approach is to discuss your report with your doctor, share any ongoing symptoms, and undergo further tests if advised. With the right context, this radiological finding can serve as an early clue, guiding timely intervention and better respiratory health.
In this blog, we will discuss what bronchovascular markings are, why they sometimes appear “prominent”, normal vs. abnormal causes, conditions linked to increased markings, diagnostic significance and when to seek medical advice.
What Are Bronchovascular Markings?
In simple terms, bronchovascular markings are the visible outlines of the lungs’ airways (bronchi) and blood vessels (vascular structures). On a chest X-ray, CT scan or tomography, they appear as thin, branching, web-like lines spread throughout the lung fields. These markings represent the normal structure of the lungs, and everyone has them.
Radiologists examine their thickness, density, and pattern to determine whether they fall within the normal range or appear more pronounced than usual, which may indicate temporary changes from infections, inflammation, fluid buildup, or other conditions that require further evaluation.
A few common reasons include:
- Mild Irritation or InflammationEven something as ordinary as a recent cold or throat infection can cause the airways to become mildly irritated. When the lining of the bronchi swells, they cast a slightly stronger shadow on the X-ray. Allergies can do the same - pollen, dust, or pet dander may trigger temporary inflammation that makes the markings appear more obvious. These changes usually settle on their own once the irritation improves.
- A Bit of Congestion or Extra Blood FlowYour lungs are constantly adjusting to what your body needs. During an infection, fever, or even after intense physical activity, the blood vessels inside the lungs may carry more blood than usual. This increased flow makes them look thicker or more prominent on a scan. It doesn’t always indicate disease, sometimes it’s simply your body responding to stress, exertion, or early congestion that resolves with rest or treatment.
- Fluid or Mucus Around the AirwaysWhen the airways produce extra mucus, whether from a viral illness, allergies, or exposure to irritants, the surrounding tissues can hold more moisture. This can make the walls of the bronchi look sharper or more outlined on imaging. Think of it like tracing a line with a slightly wetter marker; the edges look clearer. Once the mucus clears, the markings often return to their usual appearance.
- Your Natural Body StructureSome people simply have lungs that show more detail. Children, teenagers, and adults who are naturally slim often have less fat and soft tissue around the chest. Because of this, the X-ray beam passes through more easily, making even normal airway and vessel lines appear more defined. In these cases, visible markings may be completely normal for that person.
- Technical FactorsNot all X-rays are identical. Small variations such as how deep a breath you took, the angle of the machine, or the sharpness of the image, can significantly change how the markings appear. A very high-quality or high-contrast X-ray may make normal structures look bolder, while slightly rotated or overexposed films can exaggerate them. Radiologists consider these technical factors before deciding whether a finding is truly significant.
In most cases, this visibility is just a descriptive note for the doctor, not a red flag. It’s one piece of information that needs to be interpreted along with your symptoms, medical history, and any other test results. Many people with more visible markings are completely healthy.
Looking For a Second Opinion From Pulmonologist? Contact the Doctors Below
Normal vs. Abnormal Causes
Normal / Benign Reasons
- Children and young adults: Their lung tissue is thinner, making markings naturally more visible.
- Thin or underweight individuals: Less chest wall fat means lung details show up more clearly.
- Imaging technique: A very sharp or high-resolution X-ray may make markings look exaggerated.
Abnormal / Pathological Reasons
- Infections (acute or chronic bronchitis, pneumonia)
- Pulmonary congestion due to heart problems
- Chronic lung diseases such as COPD, asthma, or interstitial lung disease
- Occupational exposure to dust, fumes, or allergens
- Smoking-related changes that thicken airway walls
Conditions Commonly Linked to Increased Markings
Increased lung markings on a chest X-ray can result from various temporary or chronic conditions affecting the airways, blood vessels, or lung tissue. Below are some common medical causes that can lead to this radiological finding:
1. Respiratory Infection: Viral or bacterial bronchitis, pneumonia, or even post-viral lung inflammation can temporarily increase markings. This often resolves after treatment and healing.
2. Asthma and Allergic Airway Disease: Recurrent airway inflammation can make bronchial walls thicker, showing up as prominent markings. Asthma patients may also show “peribronchial cuffing” (ring-like shadows around bronchi).
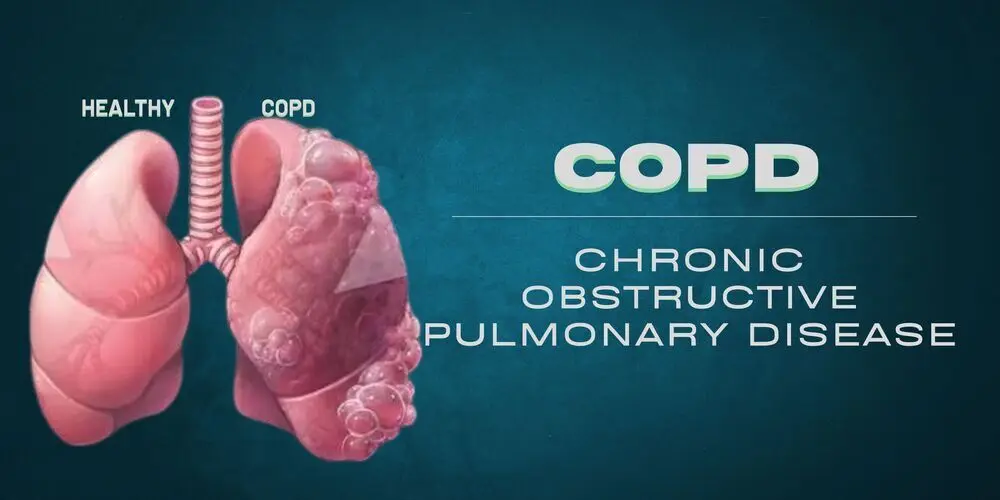
3. Chronic Obstructive Pulmonary Disease (COPD): Long-term smoking or exposure to irritants leads to structural changes in airways and vessels. Radiology often shows coarse, thickened bronchovascular markings, especially in advanced cases.
4. Pulmonary Venous Hypertension / Congestion: In heart failure or valvular heart disease, excess blood backs up into the lungs.This causes vascular markings to become more prominent, especially in the lower lung zones.
5. Interstitial Lung Disease: A group of disorders (like pulmonary fibrosis) that stiffen and scar lung tissue. Early stages may show subtle thickening of markings before progressing to more obvious changes.
6. Environmental or Occupational Lung Injury: Prolonged exposure to coal dust, asbestos, or silica can cause structural lung changes. Markings may become more defined due to inflammation and fibrosis.
Also Read:Lung Transplant in India
Symptoms That May Accompany This Finding
If prominent bronchovascular markings are associated with symptoms, they may indicate an underlying condition. Watch for:
- Persistent cough
- Shortness of breath or wheezing
- Chest pain or heaviness
- Recurrent lung infections
- Fatigue, especially on exertion
- Swelling in ankles (in heart-related causes)
Asymptomatic patients with this finding often don’t need aggressive workup unless other risk factors are present.
When Should You Be Concerned?
Not every report mentioning “prominent bronchovascular markings” is worrisome. However, you should seek medical advice if you have:
- Persistent or worsening respiratory symptoms
- History of smoking or long-term pollutant exposure
- Known heart disease, diabetes, or hypertensionFamily history of lung or cardiac conditions
- Abnormal lab tests (e.g., low oxygen, abnormal ECG, high inflammatory markers)
A doctor may recommend additional tests like a chest CT scan, pulmonary function test, or echocardiogram depending on your history.
Can They Be Prevented or Reversed?
The visibility of markings themselves isn’t usually a “disease” but a sign. Preventive strategies focus on lung and heart health:
- Quit smoking: The most effective step for reducing airway changes.
- Manage allergies & asthma: Use prescribed inhalers and avoid triggers.
- Heart health: Control blood pressure, diabetes, and cholesterol to prevent pulmonary congestion
- .Vaccinations: Annual flu shots and pneumonia vaccines reduce infection risk.
- Healthy lifestyle: Exercise, balanced diet, and maintaining healthy body weight support lung capacity.
Conclusion
Seeing the phrase “prominent bronchovascular markings” in your X-ray or CT report can feel unsettling, but in most cases, it is simply a descriptive finding rather than a definitive diagnosis. In some situations, it may indicate temporary changes from an infection, while in others, it could suggest underlying chronic lung or heart conditions that require follow-up.
The most important step is to review the report with your doctor, mention any symptoms you may be experiencing, and undergo additional investigations if recommended. Interpreted in the right clinical context, this finding can act as an early indicator, helping ensure timely care and better respiratory health.
References
- Redcliffe Labs
- Doctors Diagnostic Centre
Read More Blogs
FAQs
It refers to airways and blood vessels in the lungs appearing more visible or thicker than usual on a chest X-ray or CT scan. It is usually a descriptive finding, not a diagnosis.
They can be caused by infections, inflammation, chronic lung or heart conditions, smoking, or even normal variations related to age or body build.
There is no specific medicine for the markings themselves. Treatment targets the underlying cause, such as antibiotics for infections, inhalers for asthma, or heart medications for pulmonary congestion.
Focus on lung and heart health: quit smoking, manage asthma or allergies, maintain a healthy lifestyle, and follow medical advice for heart conditions or infections.
Consult a doctor if you have persistent cough, shortness of breath, chest discomfort, recurrent infections, or a history of heart or lung disease.
Sanjana
Author
Sanjana Sharma is a certified diabetes educator with a solid academic background in nutrition and dietetics. Her qualifications include a BSc in Clinical Nutrition and Dietetics, an MSc in Foods and Nutrition from CCS University, a Diploma in Health and Education from IGNOU, and a certification from NDEP. Dedicated to helping patients manage their health through personalized care and education, she brings expertise and compassion to her work. Outside of counseling and writing, Sanjana loves staying updated with fashion trends, sharing corporate memes on Instagram, and, of course, thinking about food.
Guneet Bindra
Reviewer
Guneet Bhatia is the Founder of HOSPIDIO and an accomplished content reviewer with extensive experience in medical content development, instructional design, and blogging. Passionate about creating impactful content, she excels in ensuring accuracy and clarity in every piece. Guneet enjoys engaging in meaningful conversations with people from diverse ethnic and cultural backgrounds, enriching her perspective. When she's not working, she cherishes quality time with her family, enjoys good music, and loves brainstorming innovative ideas with her team.